Everything we do, healthy or not, is recorded by the brain. The more we do something, the more our brain wants to continue doing that thing. This is how we’ve survived as a human species. Hundreds of thousands of years ago, the primates who were aware of their surroundings are the ones who made it through evolution and became what we are today. What protected us from predators was once useful, but now may cause us to feel unsafe in our bodies, replay traumatic events, or even more simple than that; feeling uneasy while we sit in traffic. The senses that once aided our survival were recorded by the brain and are now called anxiety.
So, how can we train the brain to overcome this feeling of worry, unease, and nervousness? Treatment may involve a few methods:
Therapy to give new light on our thoughts and behaviors
Using medication to work on the chemical base of the brain
Supportive living and immersion treatment to benefit the social aspect of our being
And neurofeedback to improve how our own electricity runs through our brain
Now, we’ve all heard of therapy and medication, but what is neurofeedback?
Neurofeedback is a method aimed at facilitating learning how to control and self-regulate your own brain activity. In a neurofeedback session, levels of brain activity from the measured area are being fed into a computer game or simulation that visually represents these activity levels. For example, if you have an overload of brain activity in the part of your brain that causes feelings of anxiety, the simulation will relay this, perhaps by causing you to lose in a video game that you are learning to control with that part of your brain, or by increasing the volume to a song you are listening to.
This feedback allows us to know how our brain activity responds in real time, which gives us the opportunity to practice mental strategies (such as breathing, meditation, counting, etc.) that influence brain activity, and to learn which mental strategy helps us the most. Imagine yourself starting to learn meditation: you sit down to relax and find yourself distracted. You get better at meditating each day you work on it but still wonder to yourself: ‘is this method I’m using to help me relax working?’ With neurofeedback, we can use that feedback to figure out exactly what works for you, and through practice and repetition, train your brain to associate this method with feeling good–or less anxious–to the point where it becomes an automatic response to stressful situations.
In my experience, I’ve primarily used neurofeedback to train others how to decrease, or ‘down-regulate’ brain activity in their amygdala.
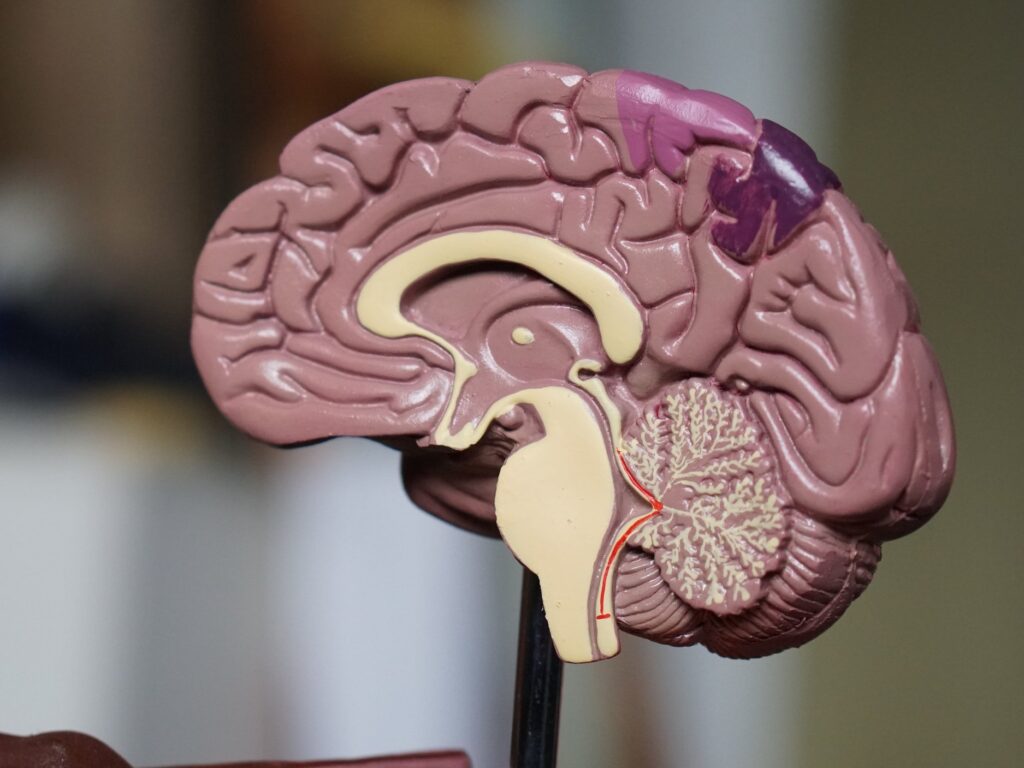
The amygdala is an almond-shaped cluster of cells, located in the lower part of our brain. It plays a role in processing our memory and emotional responses, including fear, anxiety, and the general feeling of being overstimulated. I like to think of the amygdala as a filing cabinet. When you have too much activity in your amygdala, it’s almost like your filing cabinet is disorganized and your brain is panicking to choose which file to play. This may result in flashbacks associated with post-traumatic stress, or panic as you can’t decipher how you feel about an upcoming event. By down-regulating the amygdala, we are essentially organizing our filing cabinet, helping ourselves focus on how we feel in our bodies throughout the day, rather than focusing on feelings associated with past traumas or the unexpected future.
Neurofeedback is not a new technology.
However, it’s only recently found its way into clinical practice. Although my experience is with stress disorders, anxiety, trauma, and hyperactivity associated with ADHD, neurofeedback can be used to increase brain activity in certain areas, such as the cortex, which may resolve symptoms of depression, but more on that later.
Written by: JACK SENESE IV, LCSW // THE MENTAL HEALTH COLLECTIVE’S NEUROFEEDBACK FACILITATOR
Jack specializes in both psychotherapy and research. His areas of specialization in psychotherapy include trauma, stress, PTSD, neurofeedback, substance use, and body-image concerns. As a psychotherapist, Jack has extensive experience working with LGBTQ+ individuals, veterans and survivors of trauma.
Jack’s research has focused on the neurobiology and treatment of trauma using novel methods such as neurofeedback, and the prevention and treatment of emotional and physical health outcomes in LGBTQ+ youth and adults. One of the primary health outcomes Jack’s research explores is the connection between body-image related distress with anxiety, depression, and substance use. Jack received his post-graduate psychotherapy training at the LGBTQ+ Center of Long Beach and continues to work as a research project manager at the University of Southern California.
DO YOU HAVE A QUESTION?
Send our team a message or call 888.717.9355